New Insulin Capsule Offers Needle-Free Alternative for Diabetes Patients
- Esil Korkmaz
- Feb 11, 2024
- 4 min read

Approximately 422 million people worldwide suffer from diabetes, with the rough annual death rate being 1.5 million. Insulin pens, pumps, or syringes are the main tools used in the treatment of type 1 diabetes, helping to maintain moderate blood glucose levels. If diabetes is not managed, high blood glucose levels can lead to severe complications for the kidneys, heart, eyes, nerves, and blood vessels. Insulin injections are most effective when they are taken three or four times a day, and the syringes used for injections need to be changed after two uses, which can be challenging for most type 1 diabetes patients since most of them are from middle or low-income countries. Fortunately, a new medication capsule developed by RMIT researchers has been found that can be used instead of the aforementioned treatments.
There are numerous drawbacks to insulin pens, pumps, and syringes, necessitating the development of an alternative method. Insulin pens are known for their higher cost compared to syringes, and not all insulin types are available in pen form.
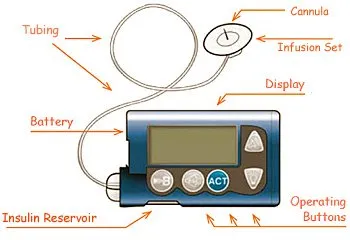
Insulin pumps, on the other hand, are even more expensive, and they require a learning period for the patient to understand the initial setup and ongoing management. Contrary to insulin pens or syringes, insulin pumps are electronic devices
that can malfunction and lead to a potential interruption in insulin delivery, which can be dangerous. Users must frequently switch infusion sites to minimize the probability of a malfunction, as failing to do so may result in irritation, infection, or issues with absorption. Insulin syringes, the most popular and widely used treatment, are no better than the other two options because they require to be refrigerated like insulin pens, and the patient must constantly carry both syringes and vials containing insulin, with the syringes needing to be changed after no more than two uses, which makes them inconvenient for most.
The newly found capsule that carries insulin aims to overcome these problems. The capsule is the size of a blueberry and contains insulin in nanocarriers, which are so small that they can’t be observed by traditional microscopes and are approximately 1/10,000th the width of a strand of human hair. In contrast to most other medicines, until now, insulin had to be injected into the body because nanocarriers that had insulin broke down in the stomach before reaching the required parts of the body. Researchers overcame this problem by creating a protective layer that prevents insulin from being digested in the digestive system and allows it to reach the liver. Because of specific enzymes, when blood sugar is high in the liver, the coating protecting insulin breaks down. As a result, insulin is released to affect the muscles, fat, and liver, and blood sugar levels are reduced. This method of taking insulin is actually more precise than insulin syringes or pens since insulin is only released to the needed parts of the body rather than being spread all through the body and causing unwanted side effects. Additionally, because it allows for controlled insulin release based on the patient's needs and reduces the risk of blood-sugar events like low blood sugar (hypoglycemia), it is more patient-friendly than injections where all the insulin is released at once. Injecting insulin results in more of it being present in muscle and fat tissues than it normally would if insulin were released by the pancreas like it would in a healthy body, which can lead to fat accumulation and hypoglycemia.
The capsule insulin has already been tested on mice, nematodes, and rats and has shown positive results. Recent trials have also been conducted on baboons in Australia’s National Baboon Colony. 20 baboons were used in the trial, and to make the capsule tastier, it was incorporated into sugar-free chocolate. After taking the medication, the blood sugars of all baboons decreased. Challenges such as weight gain, fat accumulation, and hypoglycemia that were faced with insulin injections and other types of oral medication were also not observed.
With the promising results from animal trials, the next step is to start human trials, which are expected to begin in 2025 with the help of Endo Axiom Pty Ltd. Three stages are anticipated for human trials. The first phase will focus on the safety of the medication and attempt to verify whether patients with type 1 diabetes will encounter any difficulties associated with hypoglycemia and understand how they will be able to overcome these problems. Once its safety has been established, stage two of the study will investigate whether the drug can relieve diabetic patients' need for injections. Researchers aim to make the drug available for everyone in two to three years, marking the end of phase three in human trials.
This new method for delivering insulin marks a significant threshold in offering diabetes patients a needle or injection-free alternative that is more affordable and convenient. The benefits of this method are also not limited to diabetes treatment, as researchers believe it can be used to orally deliver other protein drugs. RMIT has now filed an international patent application for their new technology, which can be revolutionary for the drug market and healthcare.
Works Cited
Banik, Dr Prajakta. “Innovative Medicine Offers a Needle-Free Life for Diabetes Patients.” Tech Explorist, 26 Jan. 2024.
RMIT. “Wonder Drug-Capsule May One Day Replace Insulin Injection for Diabetics.” Www.rmit.edu.au, 19 Apr. 2023.
WHO. “Diabetes.” World Health Organization, 2023.